Hepatitis C infection is caused by the
Hepatitis C virus (HCV), which primarily affects the liver and can lead to severe complications if untreated.
H.U.M. Clinic, a leading Sexual health clinic in Bangkok, provides both
Hepatitis C test and
Hepatitis C treatment (DAAs) to prevent long-term damage.
Hepatitis C Virus (HCV), also known as
Hep C, can be transmitted through blood and sometimes sexual contact. Individuals at risk should seek for HCV tests and other
STD test to check for other
Sexually Transmitted Infection (STI). With effective
STD treatment, including
DAA therapy, you can clear the infection and protect your health.
What is Hepatitis C?
Hepatitis C, also known as Hep C or HCV, is a viral infection that primarily affects the liver, leading to inflammation and potential long-term damage. While HCV is primarily spread through blood-to-blood contact, it can also be transmitted through sexual activity, particularly in individuals with multiple sexual partners or those with existing sexually transmitted infections (STIs).
Overview of Hepatitis C
HCV is transmitted via contaminated blood, often through shared needles, unsafe medical practices, or sexual contact with an infected person. The virus causes liver inflammation, which can lead to cirrhosis or liver failure if untreated. Unlike Hepatitis A and B, there is no vaccine available for Hep C.
Types of Hepatitis C
- Acute Hepatitis C: A short-term infection lasting up to six months, where the body may clear HCV without medical treatment.
- Chronic Hepatitis C: A long-term infection that persists for years, often leading to severe liver damage and complications if not treated properly.
Global Impact of Hepatitis C
Over 70 million people globally are infected with Hep C, with significant prevalence in regions like Asia, including Thailand. Since HCV can be transmitted through sexual activity as well as blood, early detection and treatment are crucial to prevent the spread and minimize liver damage, especially as many individuals are asymptomatic.
Hepatitis C Virus Transmission
Hepatitis C (HCV) can be transmitted through various routes, primarily via blood-to-blood contact. Understanding the key transmission methods, including bloodborne, sexual, and vertical transmission, helps in preventing the spread of this sexually transmitted infection (STI).
Bloodborne Transmission
The most common way HCV is transmitted is through exposure to infected blood. This can occur through sharing contaminated needles, unsafe medical practices, or receiving unscreened blood transfusions. Healthcare workers are also at risk of contracting Hep C through accidental needlestick injuries.
Sexual Transmission
While less common, HCV can also be spread through sexual activity, especially among individuals with multiple partners or those already infected with other sexually transmitted diseases (STDs). Engaging in rough sexual practices or sex during menstruation also increases the risk of transmission.
Vertical Transmission
Hepatitis C can be passed from mother to child during childbirth, known as vertical transmission. Although the risk is relatively low, infants born to mothers with HCV should be closely monitored and tested for the virus after birth.
Symptoms of Hepatitis C
Hepatitis C (HCV) can present with a range of symptoms, from mild to severe, depending on the stage of the infection. In many cases, Hep C may go undetected for years due to the lack of noticeable symptoms.
Early Symptoms
In the early stages, Hep C can cause nonspecific symptoms. They are often mild and can be mistaken for other common illnesses, making it difficult to diagnose without proper testing.
- Fatigue
- Nausea
- Muscle and/or Joint pain
- Malaise
Advanced Symptoms
As HCV progresses and causes more significant liver damage, more severe symptoms may develop. These signs indicate that the liver is struggling to function properly.
- Jaundice (yellowing of the skin and eyes)
- Swelling in the legs or abdomen
- Unexplained weight loss
- Dark urine
Silent Infection
Many individuals with Hep C may remain asymptomatic for years. This silent infection is a major reason why HCV often goes undiagnosed until the liver has sustained significant damage, underscoring the importance of regular testing, especially for high-risk groups.
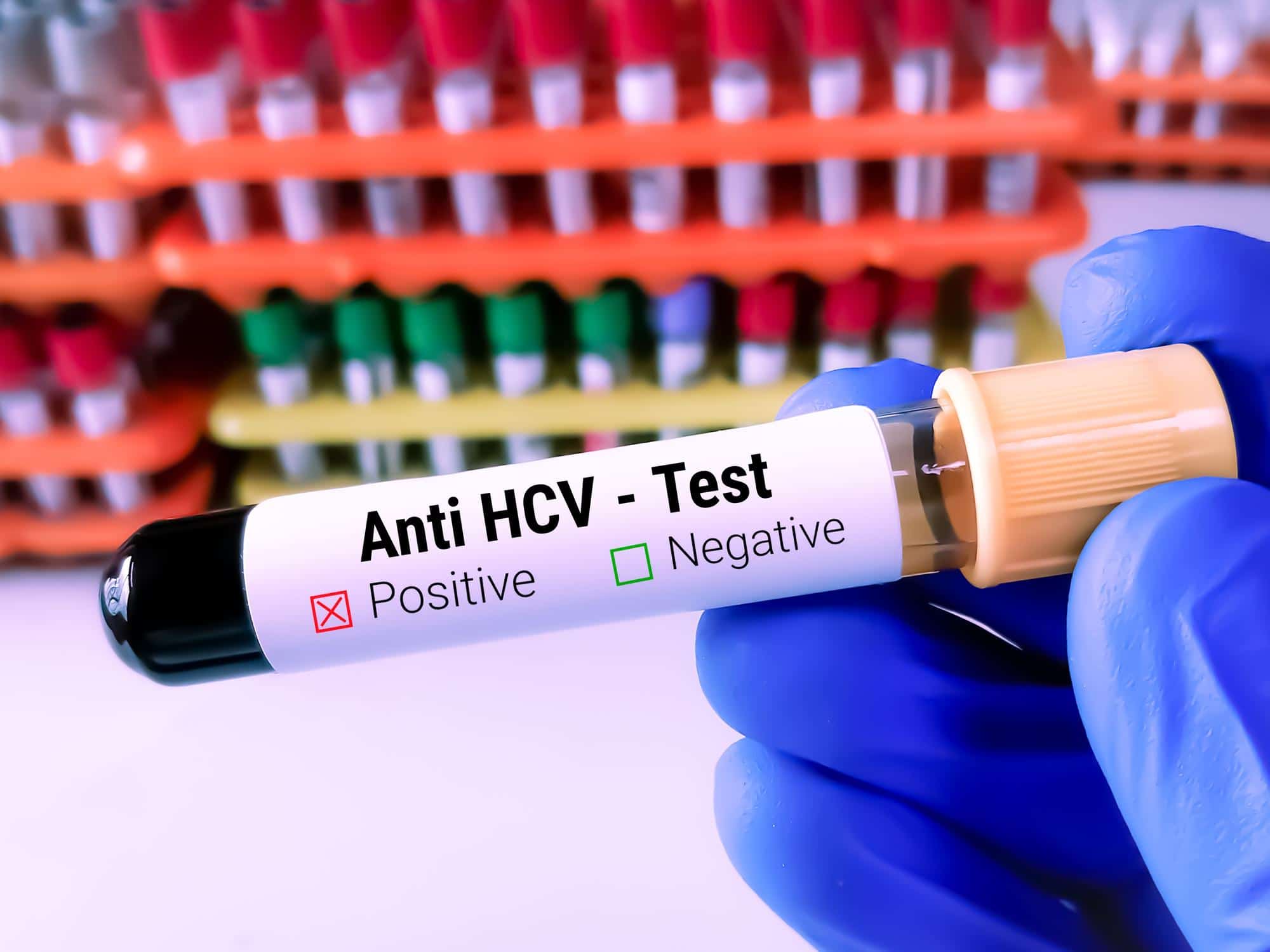
Diagnosing Hepatitis C
Diagnosing Hepatitis C (HCV) involves several tests to detect the virus and determine the course of treatment. Early diagnosis is crucial, as it helps prevent long-term liver damage and improves treatment outcomes.
Hepatitis C Blood Tests
Three key blood tests are used to diagnose Hepatitis C infection:
- Anti-HCV test detects antibodies produced in response to the Hepatitis C virus, indicating a past or present infection.
- Anti-HCV (rapid test) costs 490 THB, result in 20 minutes.
- Anti-HCV (CMIA) costs 790 THB, the result is in 1-2 days
- HCV RNA test confirms active infection by detecting the virus’s genetic material.
- HCV RNA test (PCR) costs 3,450 THB for 3-5 days result, and 5,950 THB for the Same day result.
- Hepatitis C antigen test. Doctors use the Hepatitis C antigen test to detect viral proteins in the blood, confirming active infection earlier than antibody tests.
- HCV Antigen test (CMIA) costs 2,450 THB. The result is in 1 day.
- HCV Combo Ag/Ab (CMIA) costs 2,750 THB. The result is in 1 day.
Hepatitis C Genotyping
Identifying the Hepatitis C genotype is crucial for determining the best treatment plan. Different HCV genotypes respond to antiviral medications differently, so knowing the specific genotype ensures personalized and effective treatment for each patient.
Screening Recommendations
Regular screening is recommended for high-risk individuals, including those who use intravenous drugs, received blood transfusions before 1992, or have been diagnosed with other sexually transmitted infections (STIs). Routine testing is also advised for those in ongoing high-risk situations.
Hepatitis C Treatment
Treatment for Hepatitis C (HCV) has advanced significantly in recent years, offering effective options to cure the infection. The use of modern antiviral therapies has dramatically improved patient outcomes, making Hep C highly treatable.
Antiviral Medications
The most effective treatment for Hep C is Direct-Acting Antivirals (DAAs), which target the virus directly and prevent it from replicating. One commonly prescribed DAA is Sofosbuvir/velpatasvir 400/100 mg, a combination that works against all major HCV genotypes. DAAs, including Sofosbuvir/velpatasvir, have a high cure rate of over 95% and are well-tolerated with fewer side effects compared to older treatments like interferon.
Price for Original Sofosbuvir/Velpatasvir (Sof/Vel) can be expensive (up to 100,000 THB per course) limiting access for many patients. However, generic versions of Sof/Vel offer a more affordable and accessible option, providing the same efficacy at a fraction of the cost, making treatment widely available. H.U.M. Clinic has the generic Sof/Vel regimen available. Contact us for more information.
Treatment Duration
The typical treatment duration for Hepatitis C lasts between 8 to 12 weeks, depending on the patient’s health and the specific HCV genotype. In many cases, patients can achieve a complete cure within this timeframe if they adhere to the prescribed treatment plan.
New and Emerging Treatments
New treatments and therapies for HCV are continually being researched and developed. Advances such as shorter treatment courses and drugs that are effective against all HCV genotypes are showing promise in further improving cure rates and simplifying treatment.
Prevention of Hepatitis C Infection
Preventing the spread of Hepatitis C (HCV) requires understanding how the virus is transmitted and taking steps to minimize exposure. While there is no vaccine for Hep C, several preventive measures can help reduce the risk of infection.
Reducing Bloodborne Exposure
Since HCV is primarily spread through blood, reducing exposure to contaminated blood is key. Safe needle practices, sterilizing medical equipment, and thorough screening of blood donations are essential for minimizing transmission, especially in healthcare settings and among individuals who use intravenous drugs.
Sexual Transmission Prevention
Although less common, HCV can be transmitted sexually, particularly in high-risk groups. To reduce this risk, practicing safe sex by using condoms and limiting the number of sexual partners is important. Individuals with other sexually transmitted infections (STIs) may be at higher risk of contracting Hep C.
Vaccines and Future Prevention
Currently, there is no vaccine for Hepatitis C, but research is ongoing. Scientists are working to develop a vaccine that could help prevent HCV infection in the future. In the meantime, preventive strategies focus on raising awareness and promoting safer practices to reduce the spread of the virus.
Complications of Untreated Hepatitis C
When Hepatitis C (HCV) is left untreated, it can lead to serious health complications, primarily affecting the liver but also impacting other parts of the body. Timely treatment is essential to avoid these long-term issues.
Liver Cirrhosis
A long-term HCV infection can cause liver inflammation and scarring, leading to cirrhosis. Over time, this scarring interferes with normal liver function, potentially resulting in liver failure. Cirrhosis often develops after years of untreated Hep C, emphasizing the importance of early diagnosis.
Liver Cancer
If Hepatitis C progresses without treatment, the risk of developing hepatocellular carcinoma (HCC), a type of liver cancer, increases significantly. Individuals with cirrhosis are at the highest risk of developing HCC, making ongoing monitoring crucial for those with chronic HCV.
Other Health Complications
Untreated Hep C doesn’t just affect the liver—it can also lead to diabetes, kidney disease, and other complications. Chronic HCV can weaken the body’s immune system, making it harder for the body to fight off infections. This delayed immune response, along with other metabolic disruptions, heightens the risk of additional health problems.
Living with Hepatitis C
For those diagnosed with Hepatitis C (HCV), managing the infection requires lifestyle adjustments and ongoing monitoring. With proper care and support, individuals can maintain a high quality of life while managing the virus.
Lifestyle Modifications
To prevent further liver damage, those living with Hep C should adopt a healthy lifestyle. This includes eating a balanced diet, avoiding alcohol completely, and maintaining a healthy weight. Regular medical checkups are also essential to monitor the progression of the disease and prevent complications.
Monitoring Liver Health
For individuals with chronic Hepatitis C, regular liver function tests and imaging, such as ultrasounds or elastography, are crucial. These tests help detect early signs of liver damage, such as cirrhosis or liver cancer, ensuring timely intervention if needed.
Regular Screening Tests
Even after successful treatment of HCV, reinfection is possible. The Anti-HCV test will remain reactive, but regular screening for HCV Antigen or HCV Viral Load is essential to detect reinfection. It is recommended to undergo screening every 6-12 months to ensure early detection and prompt treatment if reinfection occurs.
FAQ About Hepatitis C
Can Hepatitis C clear up on its own? 15-45% of individuals clear HCV spontaneously within the first 6 months of acute infection. The immune system’s ability to clear the virus naturally depends on various factors, including the individual’s genetic background, sex (women are more likely to clear the infection), and immune response. The rate of spontaneous HCV clearance is significantly lower in the individuals with HIV and HCV co-infection, typically around 5-25%.
How long does it take for Hepatitis C symptoms to appear? Hepatitis C symptoms may take weeks to months to appear after exposure. Some people develop symptoms within 2 to 12 weeks, while others may not show any symptoms for years, leading to a “silent infection” that damages the liver over time.
Can people transmit Hepatitis C through casual contact? People do not spread Hepatitis C through casual contact like hugging, sharing utensils, or touching. The virus spreads primarily through blood-to-blood contact, such as sharing needles or exposure to infected blood.
Do people transmit Hepatitis C as a Sexually Transmitted Infection (STI)? While Hepatitis C (HCV) primarily spreads through blood, people can also transmit it through sexual contact, especially in high-risk scenarios. However, sexual transmission occurs less often than bloodborne transmission. Individuals with multiple partners, those who engage in rough sexual practices, or those already infected with other Sexually transmitted infections (STIs) are at a higher risk.
Are there any vaccines for Hepatitis C? Currently, there is no vaccine for Hepatitis C. While research is ongoing, preventive measures like avoiding bloodborne exposures and practicing safe sex are the best ways to reduce the risk of infection.
This article was written by
Waset Thongrak, M.D.